
Signs of Drug-Induced Psychosis
The word psychosis can be daunting and scary for many people. Yet, nearly half of cocaine abusers or cannabis addicts report experiencing psychotic symptoms during withdrawal.

The word psychosis can be daunting and scary for many people. Yet, nearly half of cocaine abusers or cannabis addicts report experiencing psychotic symptoms during withdrawal.

Could you be struggling with Substance-Induced Anxiety Disorder? Learn how it develops, how is it treated, and how it’s connected with addiction.
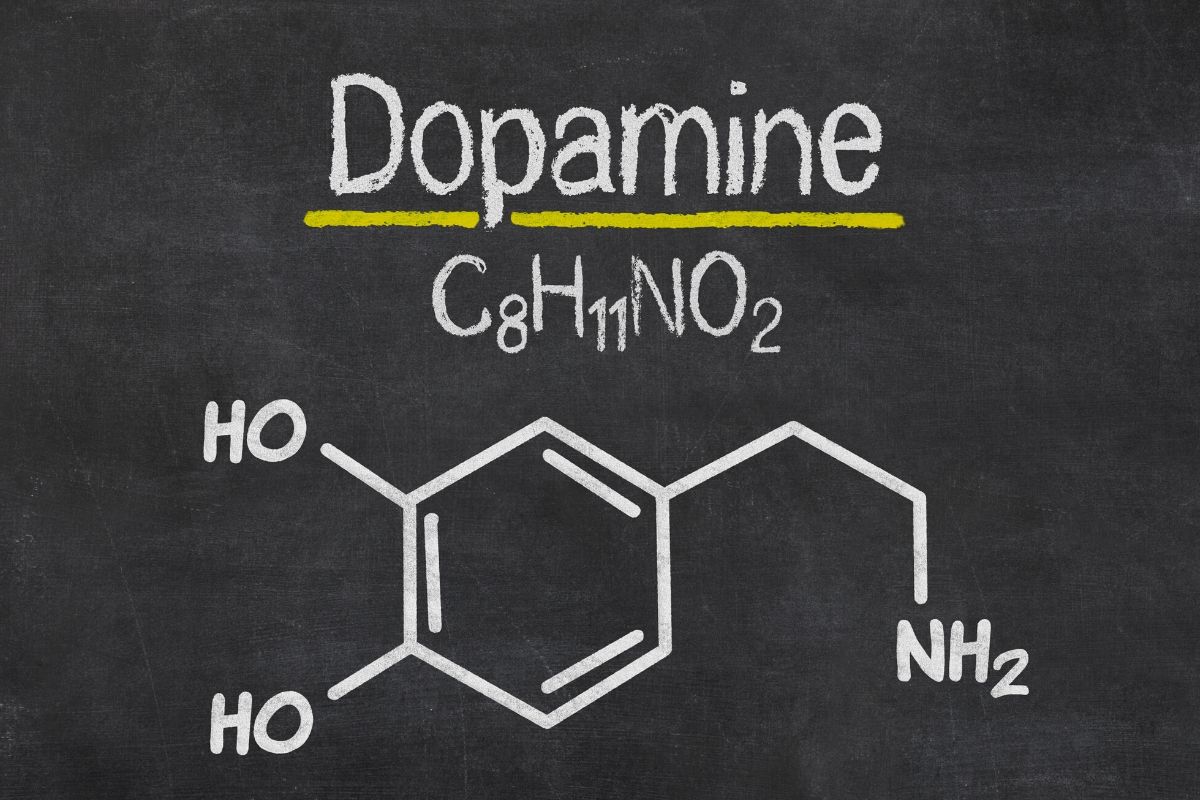
Dopamine is a naturally occurring neurotransmitter that sends signals to and from the parts of the brain that control our focus and mood and several
866-308-2090
1609 S Congress Ave
Boynton Beach, FL 33426
Lighthouse Recovery Institute treatment center is close to the beaches in gorgeous Boynton Beach, FL, Learn more